
Efficacy
Reading time: 7 min
ExteNET is a large trial designed to investigate the efficacy of extended adjuvant NERLYNX® after trastuzumab-based therapy in HER2+ early breast cancer
ExteNET study is a randomised phase III trial evaluating the addition of 1 year of NERLYNX® after trastuzumab therapy in HER2+ early breast cancer.#,1-4 Patients were treated with chemotherapy and trastuzumab. At the time of the ExteNET trial patient recruitment, pertuzumab and trastuzumab emtansine (TDM-1) were not available for adjuvant treatment in HER2+ early breast cancer. Patients included in the ExteNET trial only received prior trastuzumab.1
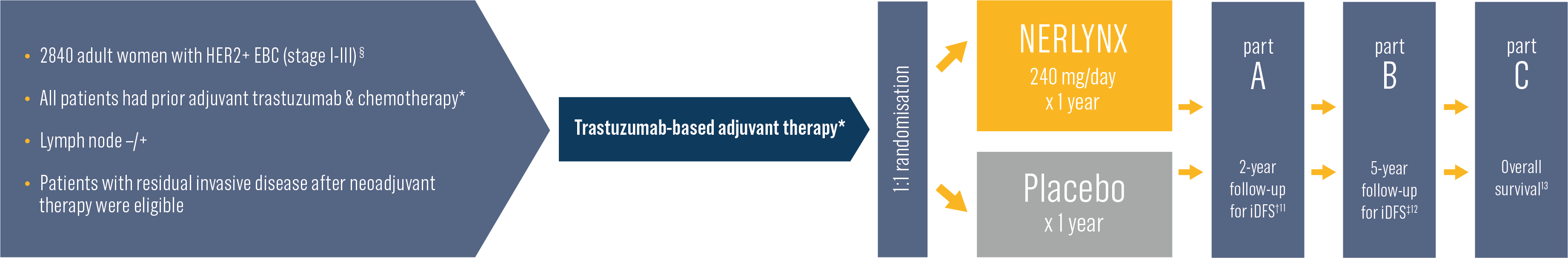
Primary endpoint
invasive disease-free survival (iDFS) at 2 years after randomisation*
Secondary endpoints
DFS-DCIS, time to distant recurrence, distant DFS, cumulative incidence of first occurrence of CNS recurrences, overall survival, safety
Other analyses
biomarkers, health outcome assessment (FACT-B, EQ-5D)
Stratification by
nodal status, HR status, concurrent vs sequential trastuzumab adjuvant regimen
NERLYNX® significantly improves invasive disease-free survival (iDFS) vs placebo in patients with HER2+ early breast cancer2,3,5
ExteNET study met its primary endpoint and demonstrates the benefit of adding NERLYNX® after a trastuzumab-based therapy for patients with HER2+ early breast cancer (ITT population, n=2840).5
iDFS after adjuvant therapy at 2 years: 94.2% vs 91.9% NERLYNX® vs placebo; absolute benefit 2.3%.
33% relative reduction in the risk of disease recurrence* vs placebo in patients with HER2+ early breast cancer.5
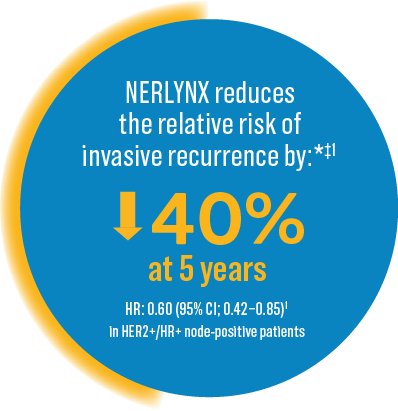
NERLYNX® shows superior benefit in patients with HER2+/HR+ early breast cancer who have completed trastuzumab-based therapy less than 1 year ago, granting marketing EU authorisation in this specific population*†‡1,5
Invasive disease-free survival (iDFS) in HER2+/HR+ ≤ 1-year from completion of prior trastuzumab-based therapy population (n=1334)
Some patients are at a heightened risk of recurrence*1,6-8
Risk considerations in early-stage HER2+ breast cancer patients
-
One or more positive nodes6
-
Tumor diameter ≥ 2cm8
-
Residual disease after neoadjuvant treatment1,7,8
-
High Ki-67†
-
HR-status1

Anna, pre-menopausal patient
with node-positive disease
Following surgery and adjuvant trastuzumab-based therapy together with endocrine therapy, Anna is disease-free

Sofia, postmenopausal non-pCR patient
following neoadjuvant treatment
Sofia has undergone a number of cycles of neoadjuvant therapy, surgery and adjuvant therapy
NERLYNX® can help reduce Anna’s risk of recurrence*1,4,6
Anna Node-positive patient
For HER2+ node-positive patients, like Anna, the risk of recurrence increases with the number of lymph nodes involved:*
- 1-3 nodes involved: 25% relapse
- ≥4 nodes involved: 45% relapse
at 10 years following 1 year trastuzumab*†6
See ExteNET study results in the node positive subgroup of patients
NERLYNX® can help reduce Sofia’s risk of recurrence*1,4,7
Sofia Non-pCR patient after neoadjuvant treatment
For patients like Sofia, who did NOT achieve a pCR and received trastuzumab-DM1, the recurrence rate is:
-
9.3% at 3 years following 41 weeks of T-DM1*†7
In descriptive analysis of patients who did not achieve a pCR after trastuzumab-based adjuvant therapy, NERLYNX® demonstrates an absolute benefit vs placebo:‡1,4
In ExteNET study, patients were treated with trastuzumab, not with T-DM1 since T-DM1 was not available at that time.










